Standards are required in many of the activities that we undertake on a day-to-day basis, whether it be the provision of a service in a hospital, or in the development of code for any software application.
The Australian Council on Healthcare Standards is involved in the accreditation of hospitals and healthcare organisations in Australia, Hong Kong, Macau, People’s Republic of China, India, Sri Lanka, Bahrain, Saudi Arabia, UAE and Qatar. The criteria that these health organisations are required to meet have been established by the Australian Commission on Safety and Quality in Healthcare (NSQHS). The ten standards provide a nationally (and in fact, internationally) consistent statement about the level of care consumers can expect from health service organisations. In the case of the ten National standards, they are:
- Standard 1: Governance
- Standard 2: Partnering with Consumers
- Standard 3: Preventing and Controlling Healthcare Associated Infections
- Standard 4: Medication Safety
- Standard 5: Patient Identification and Procedure Matching
- Standard 6: Clinical Handover
- Standard 7: Blood and Blood Products
- Standard 8: Preventing and Managing Pressure Ulcers
- Standard 9: Recognising and Responding to Clinical Deterioration in Acute Health Care
- Standard 10: Preventing Falls and Harm from Falls
The above focus is clearly on clinical services, which would be well understood by all potential patients. If a health organisation chooses to include the additional five standards as part of the accreditation process that were created by the Australian Council on Healthcare Standards (ACHS) and referred to as the EQUiP Standards, many corporate functions including IT, would be part of the formal accreditation review. The additional standards include:
- Standard 11: Service Delivery
- Standard 12: Provision of Care
- Standard 13: Workforce Planning and Management
- Standard 14: Information Management
- Standard 15: Corporate Systems and Safety
More information can be found at www.achs.org.au/media/67054/achs_web_version_v4.pdf
The first international standard for IT service management was developed in 2005 by ISO/IEC JTC1/SC7 and revised in 2011. The objective of the standard was to reflect best practice guidance for IT service management frameworks.
Wikipedia have described ISO/IEC20000-1:2011 Part 1 standard as including “the design, transition, delivery and improvement of services that fulfil service requirements and provide value for both the customer and the service provider”. Other parts of the standard, eg 20000-2 “provide guidance on the application of service management systems”, 20000-3 “provides guidance on scope definition, applicability and demonstration of conformance for service providers”, 20000-4 “is intended to facilitate the development of a process assessment model” and 20000-5 “is an exemplar implementation plan providing guidance to service providers on how to implement a service management system”.
The ISO standards are comprehensive, but may be described by some as being overly complicated.
From the perspective of Health ICT/IT, there are a number of standards that are applicable in addition to ISO above, and these include:
- HL7: is a messaging standard, which “specifies a number of flexible standards, guidelines and methodologies by which various healthcare systems can communicate with each other”.
- Dicom: is a standard “for handling, storing, printing and transmitting information in medical imaging”.
ICT Healthcare Standards
The above are standards that within the high level ICT framework standards, but there are two other standards worth mentioning that health organisations may apply for accreditation, in addition to the option of complying with the ISO standard. These are:
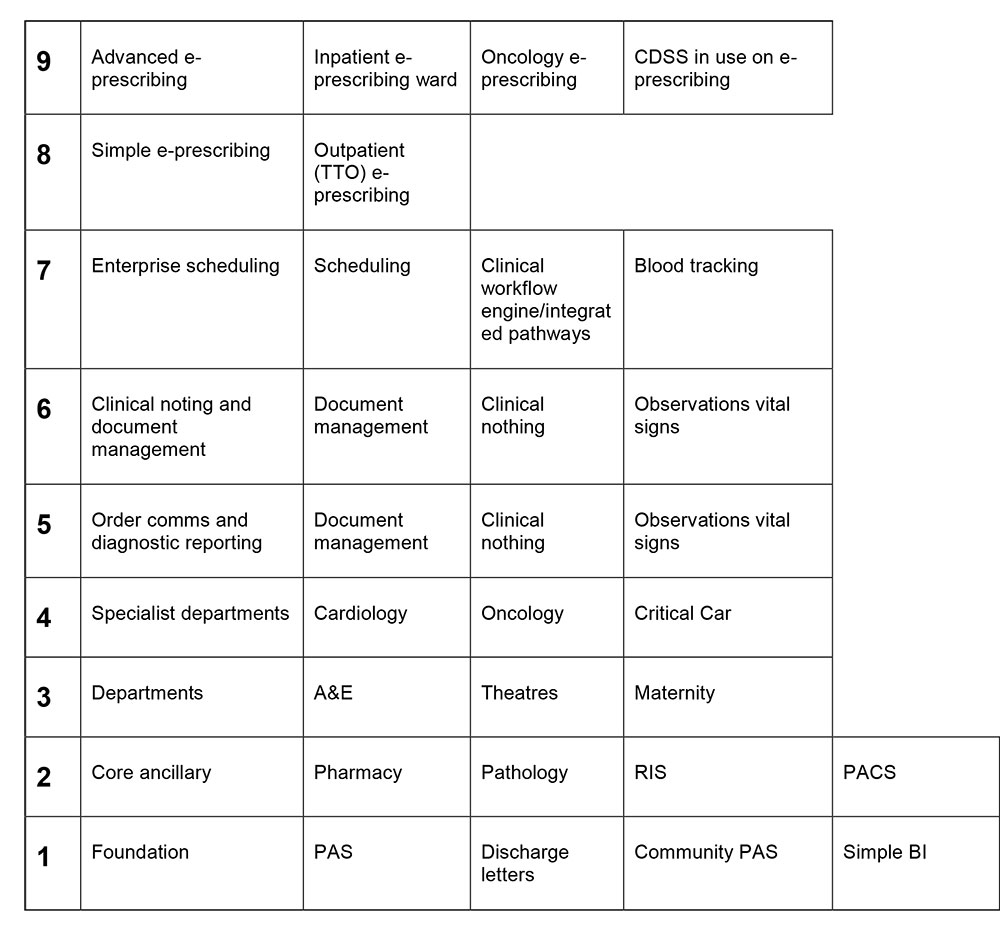
The Clinical Digital Maturity Index (CDMI)
The CDMI (Appendix A) was developed by EHI Intelligence in partnership with the National Health Service in England. It is described as providing “a unique benchmarking tool that enables NHS Trusts to better understand how investing in, then effectively using, information technology can achieve better patient outcomes, reduce bureaucracy, improve patient safety and deliver efficiencies.” The tool was launched on 5 November 2013 as an initial baseline analysis of the capability of all acute providers in the NHS. The objective was to demonstrate to Boards, clinicians and senior managers, the benefits of the investment in IT.
The NHS has since ranked hospitals against CDMI, which is available (www.ehi.co.uk/ehi-intelligence/ for all to review. Through a subscription service, the participating hospital may receive detailed information regarding their IT performance in specified areas like (1) Financial information (2) infrastructure (3) Patient Administration System (4) Order Communications and (5) Diagnostic Reporting.
The CDMI model is quite new in the UK, however, it is designed for UK purposes enabling the NHS hospitals to measure the effectiveness of their investment in IT, and through a subscription service, is able to receive advice on areas that require further investment.
HIMSS Analytics Electronic Medical Record Adoption Model (EMRAM)
I wrote in detail about the internationally recognised HIMSS Analytics Electronic Medical Record Adoption Model (EMRAM) and its use by a number of countries, in the 13 May 2014 edition of Sláinte Healthcare’s online Insights. Further and more recent achievements with the use of this model to measure the value of health organisations investment in ICT, have been published this month on himssanalytics.org. These show improvements in the achievements in the higher stages of the EMRAM model, between quarter 1 of 2014 compared with quarter 4 in 2013, but drops in other Stages of EMRAM. (Appendix B). This may obviously occur where organisations are progressing up the EMRAM model to a higher stage of achievement.
Conclusions
It is virtually impossible to determine the compliance with any particular standard. The HIMSS Analytics Adoption Model review in the US is possibly the closest that any group is able to provide such a compliance model, and the NHS CDMI ranking of 159 hospitals gives some indication of compliance.
In conclusion, organisations – healthcare and non-healthcare – may use standards as a method of ensuring that essential criteria is included in the organisation’s investment, be it in the development of software, in the provision of a service in healthcare, and in the creation of a message sharing information between organisations. No one standard is likely to meet the requirements of all internationally. I am sure that readers will agree that it is more important that we as software developers, providers of health treatments etc. seek to comply with specified criteria and standards, rather than deliver using our own internally decided standards?
Certainly we can expect that standards will continually develop and expand, to meet increasing demands and expectations of providers and consumers. We have no option but to engage and be involved with relevant standards as they evolve, if we are to progress as a service providers in the health industry.
Dr Jean Evans - eHealth Consultant
APPENDIX A: THE CDMI MODEL
APPENDIX B: UNITED STATES EMR ADOPTION MODEL (EMRAM)